Heart disease is often misconceived as a condition that predominantly affects men. However, it stands as the leading cause of death for women worldwide, presenting unique risks and symptoms that can differ significantly from those experienced by men. Understanding these distinctions is crucial for the early detection, prevention, and treatment of heart disease in women. This article explores the unique aspects of heart health in women, including risk factors, symptoms, and effective prevention strategies.
Understanding the Unique Risks
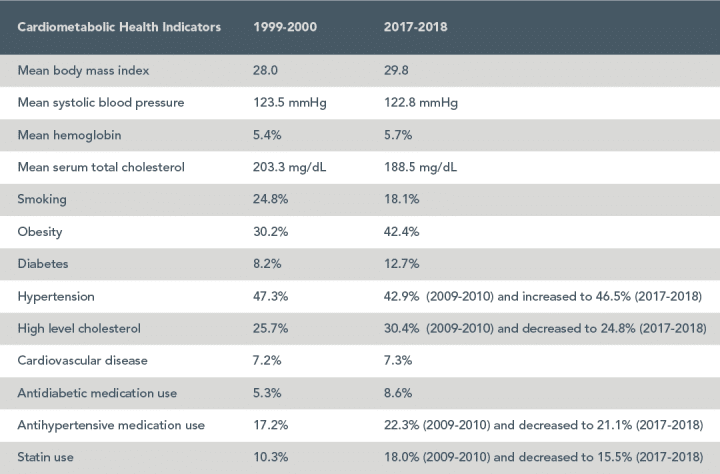
Several factors contribute to the increased risk of heart disease in women, some of which are common to both genders, such as high blood pressure, high cholesterol, obesity, and smoking. However, women face specific challenges that can elevate their risk, including:
- Menopause: The decline in estrogen levels during menopause can increase the risk of developing cardiovascular diseases due to changes in blood pressure, cholesterol levels, and blood vessel health.
- Pregnancy Complications: Conditions such as gestational diabetes and preeclampsia during pregnancy can have long-term effects on heart health.
- Autoimmune Diseases: Women are more likely to develop autoimmune conditions, such as rheumatoid arthritis and lupus, which can increase heart disease risk.
Recognizing the Symptoms
Symptoms of heart disease in women can also differ from the classic symptoms experienced by men. While chest pain is a common symptom for both genders, women are more likely to experience subtle symptoms that may be overlooked, including:
- Shortness of breath
- Nausea or vomiting
- Back or jaw pain
- Dizziness or fainting
- Fatigue
These symptoms, especially when they occur during everyday activities or rest, should prompt immediate medical attention.
Prevention Strategies
Preventing heart disease in women involves addressing the unique risk factors and adopting a heart-healthy lifestyle:
- Regular Check-ups: Regular visits to a healthcare provider for blood pressure, cholesterol, and diabetes screening can help detect potential issues early.
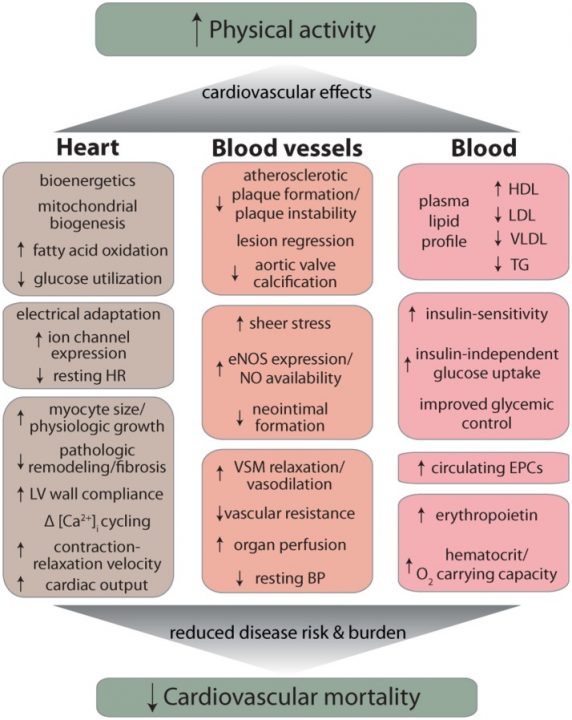
- Physical Activity: Engaging in at least 150 minutes of moderate aerobic activity or 75 minutes of vigorous activity each week can significantly reduce heart disease risk.
- Healthy Diet: A diet rich in fruits, vegetables, whole grains, lean protein, and healthy fats can help maintain a healthy weight and reduce heart disease risk.
- Stress Management: Chronic stress can negatively impact heart health. Techniques such as meditation, deep breathing, and yoga can be effective stress reducers.
- Avoid Smoking and Limit Alcohol: Smoking cessation and moderating alcohol intake are critical steps in reducing heart disease risk.
Conclusion
Heart health in women requires special consideration due to unique risk factors and symptoms. By understanding these differences, women can take proactive steps toward preventing heart disease. Regular medical check-ups, lifestyle changes, and awareness of the symptoms are key components of a heart-healthy approach. Empowering women with knowledge and resources to address heart health can lead to earlier detection, more effective treatment, and ultimately, a reduction in heart disease-related mortality among women.