Peak Heart & Vascular
Multispecialty Cardiovascular Group located in Laveen, Surprise, Avondale, Phoenix, and Flagstaff, AZ
As many as 6 million Americans have an irregularity, or arrhythmia, in their heartbeat. The team at Peak Heart & Vascular is highly skilled in diagnosing and treating the root cause of an arrhythmia. They offer compressive diagnostic testing in-office at their Laveen, Surprise, Avondale, Flagstaff, or Phoenix, Arizona, locations to identify the cause of your arrhythmia and irregular heartbeat. They offer custom treatment plans to prevent a worsening of your condition and ensure improvement in quality of life. Learn more about testing options for arrhythmias today by calling the offices or booking an appointment conveniently online.
Arrhythmia Q & A
What is an arrhythmia?
An arrhythmia is a condition that affects the rate or rhythm of your heartbeat. Your heart may beat too fast (tachycardia), too slowly (bradycardia), or with an irregular pattern.
One of the most common types of arrhythmia is atrial fibrillation, a condition that causes an irregular, fast heartbeat due to irregular contractions of the upper chambers of your heart.
Some arrhythmias are benign, but others are dangerous and life-threatening which can cause sudden cardiac death.
Other types of arrhythmias include:
- Premature atrial or ventricular contraction, or early heartbeat
- Inappropriate sinus tachycardia/POTS
- Supraventricular tachycardia (SVT)
- Atrial fibrillation
- Atrial flutter
- Ventricular tachycardia (VT) which is an abnormally fast heart rate from the lower chamber of the heart
- Ventricular fibrillation, or irregular contraction of lower heart chambers
You may also develop other types of arrhythmias depending on your health and whether you have underlying medical issues.
What causes arrhythmias?
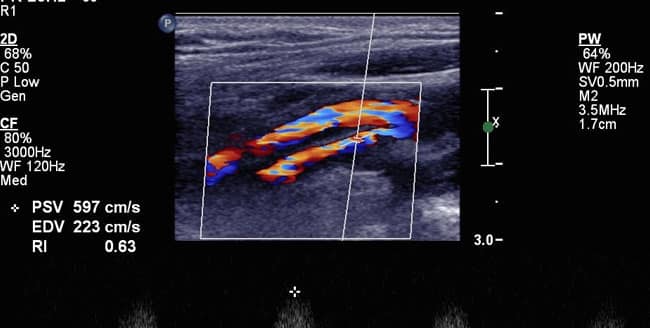
In a healthy heart, you experience 60 to 100 beats a minute. Electrical signals start in the atrium and down into the ventricles, triggering your heartbeat.
Arrhythmias are the result of interference or dysfunction in the electrical impulses of your heart. This leads to disruption in your normal blood flow to the rest of your body because your heart isn’t pumping as efficiently. This causes a variety of symptoms due to the lack of blood to your brain, lungs, and other organs.
What are the symptoms of arrhythmia?
In addition to a slow or fast heartbeat, you may experience episodes where your heart skips a beat. Additionally, you can have symptoms like:
- Sweating
- Chest pain
- Dizziness
- Lightheadedness
- Shortness of breath
- Palpitation
In some cases, an arrhythmia can result in occasional or frequent episodes of syncope, or fainting.
How is an arrhythmia diagnosed?
One of the most effective ways the team at Peak Heart & Vascular learns about the activity in your heart is by using a Holter monitor. This wearable device records important information about your heart rate and rhythm over the course of up to 48 hours.
They also offer tilt table testing, which evaluates changes in your heart and blood pressure when you change the angles of your body. For some, electrical evaluation of the heart may be needed. Called Electrophysiology Study, this procedure consists of your provider putting wires in the heart and evaluating electricity to diagnose the cause of the arrhythmia.
You may also undergo an echocardiogram, a noninvasive imaging test that allows the team the opportunity to evaluate the structure and size of your heart.
What treatments are available for arrhythmias?
In many cases, the team manages arrhythmias with medication and lifestyle modifications. You may need to stop or limit your use of alcohol and caffeine that can trigger an irregular heartbeat. You may also need to quit smoking and avoid very strenuous activities.
Ablation procedure has evolved as an effective way to cure arrhythmia and eliminate medication use. The team utilizes the most advanced equipment and ablation technique to cure arrhythmia. Some arrhythmias may require a defibrillator implant to prevent sudden cardiac death.
If your irregular heartbeat is the result of an underlying heart condition, the team at Peak Heart & Vascular can create a custom treatment plan to manage your condition and alleviate symptoms, including arrhythmia, and to prevent a stroke, heart failure, and death.
Don’t ignore symptoms of an arrhythmia. Schedule an evaluation at Peak Heart & Vascular today, online or by phone.