Peak Heart & Vascular
Multispecialty Cardiovascular Group located in Laveen, Surprise, Avondale, Phoenix, and Flagstaff, AZ
Congestive heart failure (CHF) occurs if your heart muscle stiffens or weakens, affecting its ability to pump blood. Unless it’s spotted early on, congestive heart failure could lead to a potentially life-threatening heart attack or cardiac arrest, so it pays to get a checkup at Peak Heart & Vascular in Laveen, Surprise, Avondale, Flagstaff, or Phoenix, Arizona. The team of board-certified cardiologists performs advanced, minimally invasive procedures like CardioMEMS™ monitor implantation and pacemaker implantation. Call Peak Heart & Vascular today to schedule a consultation or book an appointment using the online form.
Congestive Heart Failure (CHF) Q & A
What is congestive heart failure?
Congestive heart failure is a condition in which your heart is no longer pumping blood around your body as efficiently as it should. This happens when something damages your heart muscle, making it stiff or weak.
While you can continue to function like this for a while, at some point, your heart muscle becomes so severely affected it can’t pump or fill, resulting in a potentially life-threatening heart attack or cardiac arrest.
What are the symptoms of congestive heart failure?
Some common symptoms of congestive heart failure include:
- Rapid or irregular heartbeat
- Fatigue and weakness
- Swelling in your feet and ankles
- Coughing and producing blood-tinged mucus
- Nighttime urination
- Ascites (abdominal swelling)
- Fluid retention
- Nausea and loss of appetite
- Difficulties concentrating
You’re also likely to have some shortness of breath during exercise or when you’re lying down.
What causes congestive heart failure?
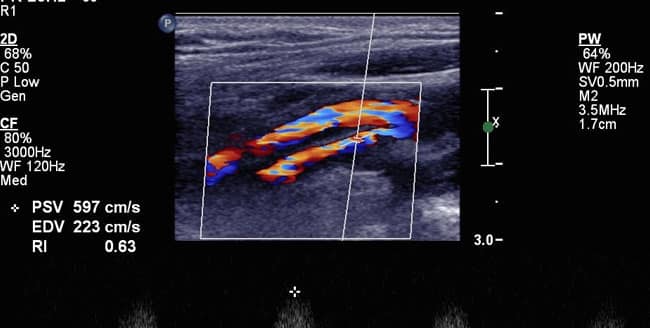
Coronary artery disease is the most likely cause of chronic congestive heart failure. With coronary artery disease, plaque formed from cholesterol and other waste products in your blood coats the inside of the arteries serving your heart, limiting blood flow.
Other causes of congestive heart failure include:
- High blood pressure (hypertension)
- Heart arrhythmias (abnormal heart rhythms)
- Valvular heart disease
- Cardiomyopathy (damaged heart muscle)
- Myocarditis (inflamed heart muscle)
- Congenital heart defects
Smoking and alcohol abuse, as well as chronic conditions such as diabetes, thyroid disease, and HIV, can also increase your risk of congestive heart failure.
Sometimes congestive heart failure happens suddenly rather than being a chronic problem. In this case, likely causes include pulmonary embolisms, heart infection, allergic reaction, and medication side effects.
How is congestive heart failure treated?
There are medications your provider at Peak Heart & Vascular can prescribe to treat your congestive heart failure. These include:
- Angiotensin-converting enzyme (ACE) inhibitors
- Statins
- Blood thinners
- Angiotensin II receptor blockers
- Beta-blockers
- Diuretics
- Aldosterone antagonists
- Inotropes
- Digoxin (digitalis)
- Nitrates
Your provider selects the most appropriate of these medicines to prolong and improve your life as much as possible based on the cause of your congestive heart failure.
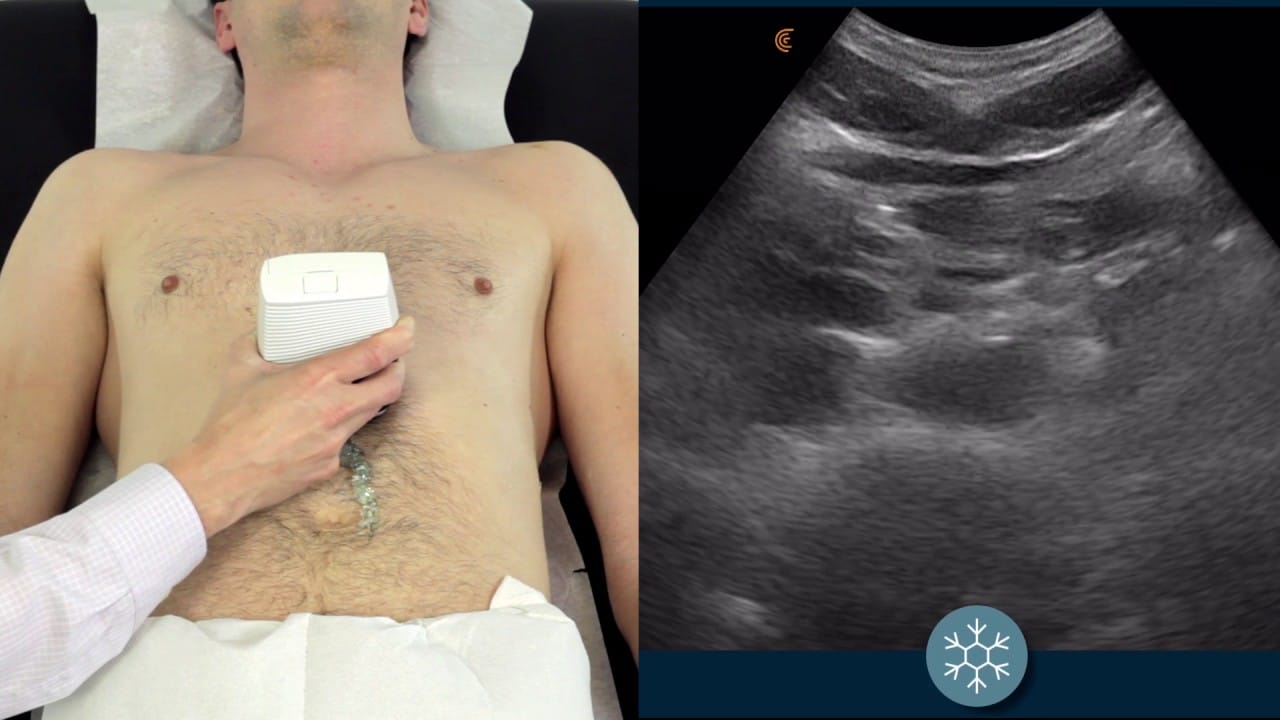
Peak Heart & Vascular also uses the cutting edge CardioMEMS HF System heart failure monitor to keep track of your condition. This implantable device detects blood pressure changes in your pulmonary artery – the main artery between your lungs and heart.
CardioMEMS relays information wirelessly to the Peak Heart & Vascular team so they can make adjustments to your medication. If your congestive heart failure is severe, you might benefit from having an implantable biventricular pacemaker, ventricular assist device (VAD), or cardioverter-defibrillator (ICD).
If you’ve been experiencing congestive heart failure symptoms, visit Peak Heart & Vascular for expert diagnosis and treatment. Call today or book an appointment online.