Peak Heart & Vascular
Multispecialty Cardiovascular Group located in Laveen, Surprise, Avondale, Phoenix, and Flagstaff, AZ
Coronary artery disease is a common heart condition that could lead to a potentially life-threatening heart attack, but it often doesn’t cause symptoms until it reaches an advanced stage. To find out whether you’re at risk, get a checkup at Peak Heart & Vascular in Laveen, Surprise, Avondale, Flagstaff, and Phoenix, Arizona. The board-certified cardiologists perform expert percutaneous coronary intervention (PCI) procedures at their ambulatory surgery center, including managing patients who have multivessel coronary artery disease. Call Peak Heart & Vascular today to schedule a consultation or book online.
Coronary Artery Disease Q & A
What is coronary artery disease?
Coronary artery disease is a circulatory problem that affects the major blood vessels supplying your heart.
The most likely cause of coronary artery disease is the build-up of cholesterol and other debris from your blood on the walls of the blood vessels. This sticky substance – known as plaque – makes the arteries narrower, resulting in restricted blood flow.
Consequently, you might experience pain in your chest and breathlessness and could suffer a heart attack.
What tests might I need for coronary artery disease?
The Peak Heart & Vascular team can perform several advanced diagnostic procedures to test for coronary artery disease, including:
Cardiac stress test
A cardiac stress test evaluates the performance of your heart when you’re exercising. You wear electrodes that record your heart’s activity on an ECG (electrocardiography) machine, just like you would for a standard ECG test.
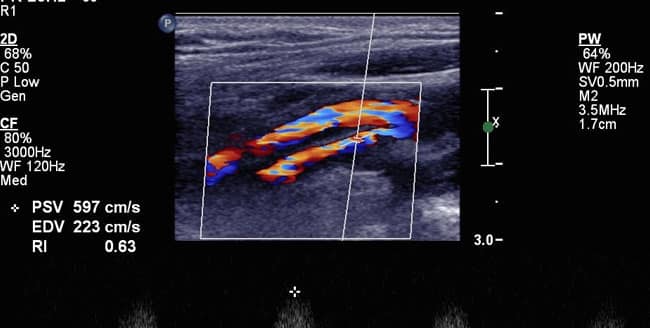
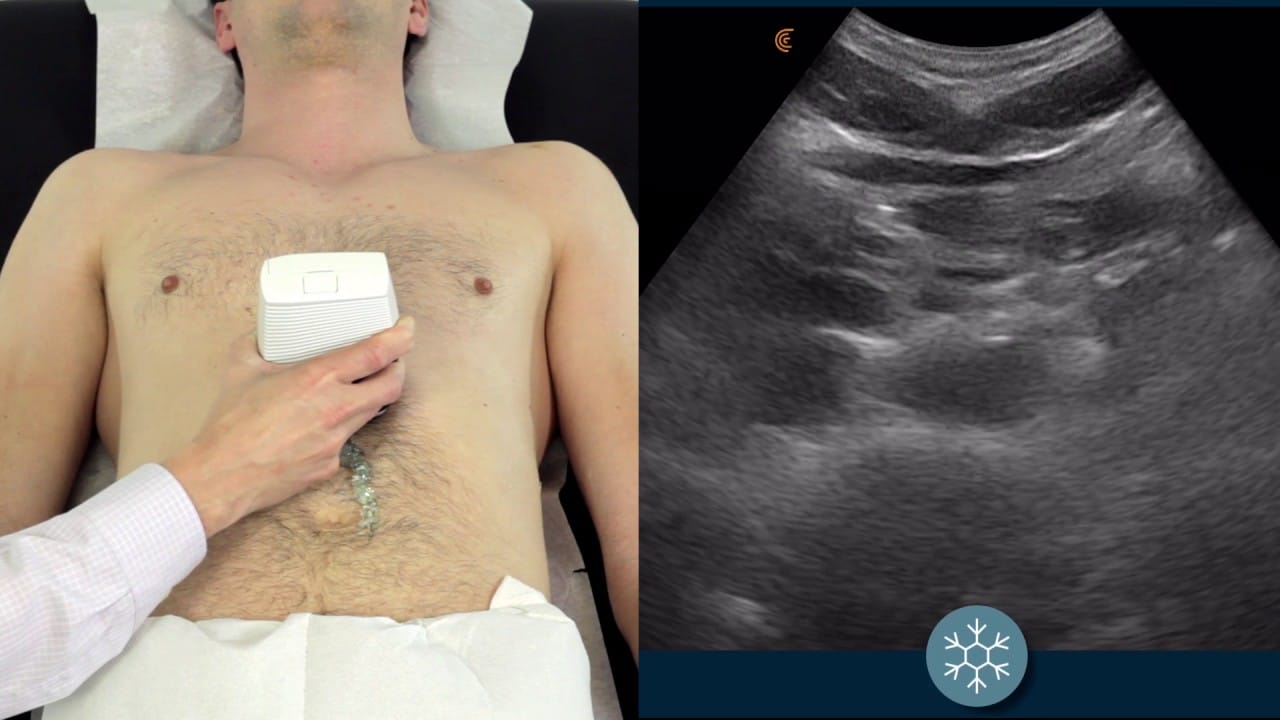
The difference is that at the same time, you raise your heart rate by exercising on a treadmill or stationary bicycle. This test can detect problems that a standard ECG might not pick up. An echo stress test is very similar but uses ultrasound technology to create detailed images of blood flowing through your heart.
Cardiac catheterization
Cardiac catheterization can both diagnose and treat heart and circulatory problems. Your provider at Peak Heart & Vascular inserts a long, slender pipe called a catheter into an artery and feeds it along the blood vessels to your heart.
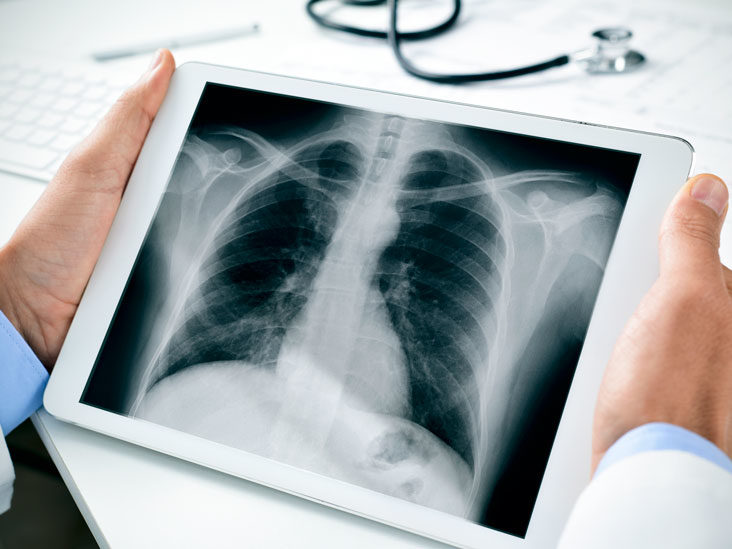
The catheter could go in your groin, neck, or arm. There are various tests you can then undergo to check your circulation. One of the most common is an angiogram, where your provider injects dye into your heart. Viewed under X-ray, the dye shows up areas where your arteries are narrow or blocked.
How is coronary artery disease treated?
The Peak Heart & Vascular team practices preventive cardiology, which means they start by looking at what aspects of your lifestyle might have contributed to the plaque build-up that caused your coronary artery disease.
The following are all likely to cause coronary artery disease:
- Being overweight or obese
- Smoking
- Lack of exercise
- High cholesterol
Tackling these problems can reverse a lot of the damage to your arteries.
You might also need to take medication, at least in the earlier stages. For example, blood-thinning medicines could help to stop your blood from forming clots that block an artery, or you could take cholesterol-lowering medication.
What interventions might I need for coronary artery disease?
If your arteries are badly blocked, you might need to undergo percutaneous coronary intervention (PCI) or coronary angioplasty. In this procedure, your provider at Peak Heart & Vascular uses cardiac catheterization techniques to put a small mesh tube (stent) into the artery. The stent squeezes the plaque flat to open up the artery and prevent blockages.
Other procedures the team specializes in include transcatheter aortic valve replacement (TAVR) and transcatheter aortic valve implantation (TAVI).
The Peak Heart & Vascular team performs interventional treatment of coronary artery disease in an ambulatory surgery center (ASC) setting. Their cardiologists were not only some of the first physicians in Arizona to do so, but have shown a track record of safety with ambulatory outpatient procedures.
To make sure your coronary arteries are in good shape or for coronary artery disease treatment, call Peak Heart & Vascular today or book an appointment online.